My Home Birth Story (Video Included) – “I Wish I Knew…” Episode 10

newborn
family
Client tips
parent tips
"I wish I knew"
I'm Marjorie
LOS ANGELES NEWBORN & FAMILY PHOTOGRAPHER
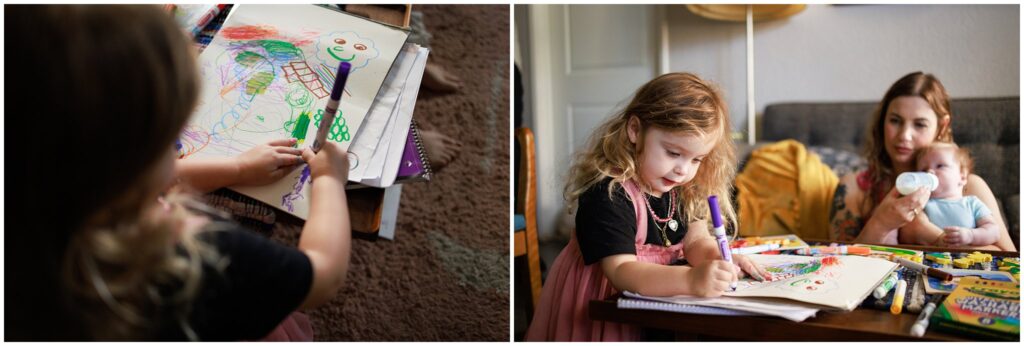
I work with parents who want relaxed and unposed photos, providing them with images that capture the joyful and unscripted moments in life.
More about Me
In this episode of the parenthood documentary series, “I Wish I Knew,” Marina recounts her out-of-hospital birth stories, and how her chaotic and urgent hospital transfer left her with PTSD.
My Out-of-Hospital Birth Left Me With PTSD
TABLE OF CONTENTS

Marina opted to deliver her first baby with a midwife at a birth center to “embrace birth as a rite of passage,” and as a “political decision to divest from the hospital system which, I think in the US, is deeply problematic.”
After having the perfect water birth and welcoming her baby daughter, Marina was diagnosed by her midwife with retained placenta. The midwife attempted to scoop out the placenta at the birth center, which proved to be excruciatingly painful. Marina was then rushed to the hospital in an ambulance to get her placenta surgically removed.
Her experience there was chaotic, as she was put under general anesthesia without her consent, and later had to be separated from her hours-old infant during her overnight stay in order to receive a blood transfusion.
Marina’s hospital stay left her with post-traumatic stress disorder (PTSD,) which she later addressed with the help of a therapist. Thankfully, the birth of her second child, which took place at home, happened safely and without any medical issues.
Check out the episode to hear the full story.

Out-of-Hospital Birth
“Since the 1970s, most births in the United States have been planned to occur in a hospital. However, a small percentage of Americans choose to give birth outside of a hospital. The number of out-of-hospital births has increased, with one in every 61 U.S. births (1.64%) occurring out of the hospital in 2018.
Out-of-hospital (or community) birth can be planned or unplanned. Of those that are planned, most occur at home and are assisted by midwives.
Patients who choose a planned community birth do so for multiple reasons. Planned community birth is associated with decreased odds of obstetric interventions, including cesarean delivery. Perinatal outcomes for community birth may be improved with appropriate selection of low-risk, vertex, singleton, term pregnancies in patients who have not had a previous cesarean delivery.
A qualified, licensed maternal and newborn health professional who is integrated into a maternity health care system should attend all planned community births. Family physicians are uniquely poised to provide counseling to patients and their families about the risks and benefits associated with community birth, and they may be the first physicians to evaluate and treat newborns delivered outside of a hospital.”
For more information and resources on out-of-hospital birth, please visit the link below.
Source: American Family Physician

US Maternal and Infant Mortality Rate
“The United States has the highest infant and maternal mortality rates out of any other high-income country and simultaneously spends the most on health care, according to a report released Tuesday by the Commonwealth Fund.
The report evaluated US health spending, outcomes, status, and service use compared with Australia, Canada, France, Germany, Japan, the Netherlands, New Zealand, Norway, South Korea, Sweden, Switzerland, and the United Kingdom. In addition, US health system efficiency was compared with the Organisation for Economic Co-operation and Development (OECD) average of the 38 high-income countries that had available data from December 2022.
Of all countries in 2020, the United States possessed the highest infant mortality rate at 5.4 deaths per 1000 live births, which is markedly higher than the 1.6 deaths per 1000 live births in Norway, which has the the lowest mortality rate.
US maternal mortality in 2020 was over 3 times the rate in most of the other high-income countries, with almost 24 (23.8) maternal deaths for every 100,000 live births.
The authors cited a few reasons behind the danger of giving birth in the United States, including:
- Inadequate prenatal care
- High rate of cesarean section
- Poverty, which contributes to chronic illnesses like obesity, diabetes, and heart disease”
Visit the link below to read more on maternal and infant mortality rate in the United States.
Source: AJMC (American Journal of Medical Care)

Midwifery Model of Care
“The Midwives Model of Care™ is a fundamentally different approach to pregnancy and childbirth than contemporary obstetrics. Midwifery care is uniquely nurturing, hands-on care before, during, and after birth. Midwives are health care professionals specializing in pregnancy and childbirth who develop a trusting relationship with their clients, which results in confident, supported labor and birth. While there are different types of midwives practicing in various settings, all midwives are trained to provide comprehensive prenatal care and education, guide labor and birth, address complications, and care for newborns. The Midwives Model of Care™ is based on the fact that pregnancy and birth are normal life events. The Midwives Model of Care includes:
- monitoring the physical, psychological and social well-being of the mother/birthing parent throughout the childbearing cycle
- providing the mother/birthing parent with individualized education, counseling, and prenatal care, continuous hands-on assistance during labor and delivery, and postpartum support
- minimizing technological interventions and
- identifying and referring women/birthing people who require obstetrical attention.
The application of this model has been proven to reduce to incidence of birth injury, trauma, and cesarean section.”
Visit the link below to read more about midwives and the midwifery model of care.
Source: Midwives Alliance North America

Midwife vs OB/GYN
SIMILARITIES:
“Midwives and OB-GYNs are both highly trained and certified. Midwives and OB-GYNs are experts in women’s health and pregnancy care who have extensive specialty training and experience in their field. In addition, each has received a relevant certification, which means they have demonstrated knowledge and skill within their area of expertise.”
DIFFERENCES:
“OB-GYNs and midwives have different credentials and educational backgrounds. While OB-GYNs and midwives are part of the same specialty area, the training, education requirements and credentials they hold are different.
An OB-GYN – which is short for obstetrician-gynecologist – is a medical doctor who specializes in women’s reproductive health, as well as pregnancy care and delivering babies. They’re also surgically trained and can perform Cesarean sections (C-sections) when necessary. You may already visit an OB-GYN for your annual well-woman’s visit.
When it comes to training and education, OB-GYNs complete four years of medical school, a four-year residency program and a three-year fellowship.”
BIRTHING SPECIALTIES:
“OB-GYNs and midwives have different birthing specialties.
Birthing specialties are one of the most important differences between midwives and OB-GYNs. Why? Depending on your needs, certain specialized care may be required for you and your baby’s health and safety. And depending on your preferences, you may be looking for someone who has specific experience. Here are a few examples:
- High-risk vs. low-risk pregnancies – OB-GYNs can manage high-risk or complicated pregnancies such as women who are expecting twins or have preexisting medical conditions. Midwives, on the other hand, can manage low-risk pregnancies and births, but can coordinate care with other specialists like OB-GYNs if necessary.
- Water births – While water births (or tub births) are becoming increasingly common in hospital settings where OB-GYNs are the primary care provider, they are very common within the midwifery specialty. So, if you are leaning toward a midwife, chances are high that water births are among their top specialties.
- C-sections – Midwives can’t perform C-sections, whether they’re planned in advance or become needed to safely deliver your baby. OB-GYNs have the surgical training to perform scheduled, unplanned and emergency C-sections, which is one of the reasons they can handle high-risk or complicated pregnancies.”
Visit the link below to read more the similarities and differences between a midwife and an OB/GYN.
Source: Health Partners

What is a Doula?
“Doulas are trained professionals who provide physical, emotional and informational support throughout the pregnancy, birth and postpartum experience.
How doulas are different from midwives?
While doulas are trained professionals, they’re not trained health professionals like midwives. Doulas do not deliver babies, rather they provide support through the process. Midwives (and OB-GYNs) deliver babies and are responsible for the health and well-being of their patients.”
Visit the link below to read more about doulas.
Source: Health Partners
What is Retained Placenta?
“Retained placenta is when the placenta doesn’t completely come out of the uterus after the baby is born.
Sometimes, a piece of the placenta is left behind in the uterus (womb). It’s not common, but it can be serious. It can cause problems days or weeks after the birth.
Retained placenta can lead to severe infection or life-threatening blood loss for the mother.
What causes retained placenta?
Sometimes the placenta takes longer than expected to be delivered. The placenta can be retained after your baby is born if:
- your contractions aren’t strong enough to expel it
- the placenta is unusually strongly attached to the wall of the uterus
- you have placenta accreta (when the placenta implants too deeply into the wall of the uterus)
- the cervix closes and traps the placenta inside your uterus
What are the signs and symptoms of retained placenta?
Retained placenta is when the placenta doesn’t completely come out of the uterus after the baby is born.
Sometimes a piece of placenta is left behind in the uterus. If this happens, you may develop symptoms days or weeks after the birth. These may include:
- fever
- a bad smelling discharge from the vagina
- heavy bleeding
- large pieces of tissue coming out of the vagina
- pain”
Visit the link below to read more retained placenta.
Source: Pregnancy Birth & Baby

Birth Trauma (Postnatal PTSD)
“Birth trauma is a shorthand phrase for post-traumatic stress disorder (PTSD) after childbirth.
PTSD was first identified amongst soldiers returning from the Vietnam War, and most people still think of it as a condition experienced by soldiers. In fact, PTSD can follow any traumatic event – such as being in a car accident, being sexually abused or having a very difficult birth.
Symptoms of birth trauma:
- Re-experiencing the traumatic event through flashbacks, nightmares or intrusive memories. These make you feel distressed and panicky.
- Avoiding anything that reminds you of the trauma. This can mean refusing to walk past the hospital where you gave birth, or avoiding meeting other women with new babies.
- Feeling hypervigilant: this means that you are constantly alert, irritable and jumpy. You worry that something terrible is going to happen to your baby.
- Feeling low and unhappy (“negative cognition” in the medical jargon). You may feel guilty and blame yourself for your traumatic birth. You may have difficulty remembering parts of your birth experience.
Not everyone who has had a traumatic experience suffers from PTSD, but many do. It’s a completely normal response, and not a sign of weakness. It’s also involuntary: brain scans show a difference between the brains of people with PTSD and those without. PTSD is not something that can be cured by “pulling yourself together” or “focusing on the positive,” despite what other people tell you.”
Visit the link below to read more about birth trauma.
Source: Birth Trauma Association

About Marjorie
Hi, I’m Marjorie. I’m a Newborn & Family Photographer based in Los Angeles, California, and the creator of this documentary series, “I Wish I Knew… A Series on Parenthood.”

Soon after I started my business and began hanging out with different families, I realized every single parent I knew had gone through something. Everyone had a story.
I decided to use my background in filmmaking to create a platform where parents could share their stories. My hope is that we can learn from each other and normalize events and experiences that have been labeled as taboo.
Sign up to receive the latest episode!
If you’re interested in staying in the loop and being among the first to watch new episodes as they are released, join the email list!
We cover topics such as mental health, pregnancy loss, adoption, divorce, out-of-hospital birth, and more.
Preparing Your Home For Your Photo Session
Easy and stress-free guide on getting your home ready for a photo session. Here’s what you need to do and here’s what you can skip!
5 Quick Tips for
grab your guide
free guide
Post Comments